Gynecological services
- General Gynecology
- Bone Health
- Nutrition
- Vitamin D
- Sexually Transmitted Diseases
- Abnormal Bleeding
- Menopause & Hormonal Replacement
- Cancer Detection Testing
- Cervix and HPV
- Breast
- Ovary
- Uterus
- Surgeries
- Gynecological
- Cosmetic

Bone Health
Bone health is a crucial part of overall women's health. Every day, our body breaks down old bone and replaces it with new bone. From childhood until thirty years of age, bone is formed faster than it is broken down. After thirty years of age, the process reverses, and bone is broken down faster than it is made. In order to promote a healthy equilibrium, women of all ages should consume sufficient calcium and vitamin D through diet and supplementation. Together with daily exercise, women can maintain healthy bones.
Yet, many women are unaware that their bones are weak. Osteoporosis, which causes weak bones that are prone to fracture, is the most common bone disease, and is known as the "silent thief" since it progresses without symptoms or pain until bones start to break. There are many risk factors, including menopause, removal of ovaries, personal or family history of fracture, lifelong diet low in calcium, lack of exercise, use of medications such as steroids, alcohol consumption, smoking and low body weight. Osteoporosis is preventable if risk factors are detected early, and it is treatable in other cases. So long as osteoporosis or pre-osteoporosis is treated medically, people can live actively and comfortably.
When testing is necessary, painless bone mineral density tests are used. The onset of testing depends on individual risk factors, but most menopausal women should undergo testing. Bone density tests determine the presence of bone loss, the rate of bone loss and the risk of a fracture. The treatment of decreased bone density depends on the degree of bone loss. The conservative treatment is increased intake of calcium and vitamin D combined with proper exercise, while medications are reserved only for patients who have significant bone loss.
The bottom line is the prevention of bone disease. Slowing the process of bone loss helps maintain strong bones. The goal is always to keep as much bone as possible. During her assessment, the doctor will review the individual risk factors for a particular patient. Appropriate tests and recommendations will then be made.

Nutrition
Food choices greatly affect our health and well being. Medical studies show repeatedly that choosing healthy foods can help prevent cancer and other diseases. A healthy diet can also help maintain proper weight, and since being overweight substantially increases risk factors for several conditions such as coronary heart disease, diabetes, and stroke, the food choices we make are very important.
Though abundant evidence suggests that the healthiest diets reduce fats and simple carbohydrates while including large amounts of vegetables and fruits, Dr. Suarez believes strongly that a healthy diet is part of a sustainable lifestyle, not a momentary fad that is difficult or dangerous to maintain. Reducing intake of meats and sugars is a powerful step in disease prevention. These products are typically high in saturated fat and cholesterol and completely without fiber. They have also been specifically linked to an increased risk of certain types of cancers. But drastic changes are frequently difficult, and the doctor recommends instead increasing consumption of other healthy options. For example, eating a low-fat, plant-based diet rich in whole grains, beans, fruits, and vegetables is another way to prevent disease.
In her dietary assessment, Dr. Suarez obtains information in order to identify dietary components that affect individual health risks. Patients are asked to maintain a food diary and to bring it to their visit. The assessment concludes with recommendations for dietary lifestyle changes that are appropriate, attainable, and sustainable.
CORONARY HEART DISEASE
Coronary heart disease (CHD) is the leading cause of death among all women in the United States. In fact, many more women die each year from heart disease than from breast cancer. Since obesity is one of the risk factors for heart disease, diet is of utmost importance for its prevention.
The risk of heart disease increases with consumption of saturated fats such as butter and decreases with consumption of monounsaturated fats such as olive oil. In addition, women with a higher intake of fruits and vegetables, fish and poultry, and whole grains show lower incidence of CHD. Similarly, a diet low in red meats and processed meats, sweets, fried foods, and refined grains significantly lowers the risk of CHD.
-
To decrease the risk of CHD, improve your diet. In addition:
- Get treatment for medical conditions such as hypertension
- Stop smoking
- Exercise
- Limit alcohol to no more than one drink per day
- Get treatment for depression

Vitamin D
Vitamin D is found in foods such as fortified milk and fatty fish, yet the quantity of vitamin D found in food is insufficient for the body, thus the need for supplementation. You would have to drink 100 cups of milk per day in order to get enough vitamin D from milk.
-
Vitamin D deficiency is widespread. It can result from:
- Inadequate sun exposure
- Inadequate supplementation
- Inability to absorb vitamin D from intestines
- Inability to process vitamin D due to kidney or liver disease
Infants and elderly adults are at risk for low vitamin D levels because of inadequate intake and insufficient sun exposure. Breast milk contains low levels of vitamin D and most infant formulas do not contain sufficient quantities. Elderly adults often do not consume enough vitamin D rich foods and do not supplement properly. Sun exposure is not recommended for infants and children due to the potential risk of skin disease. Adults who have limited sun exposure are also at increased risk of vitamin D deficiency, especially if their skin is dark.
As we age, reduced amounts of vitamin D are made in the skin and stored in the body. Additionally, the recommended use of sunscreen limits production of vitamin D in the skin. Certain diseases such as celiac disease interfere with the ability to absorb vitamin D from the intestinal tract.
Vitamin D deficiency is common and without symptoms but can be associated with reduced bone density, decrease in blood calcium level, and acceleration of bone breakdown. All of these can increase risk of falls and possibly fractures, which can seriously affect quality of life.
It is extremely important to identify and treat vitamin D deficiency. Treatment is essential to bone health and the health of the immune, muscular and cardiovascular systems.

Sexually Transmitted Diseases (STDs)
Caused by bacteria or virus, sexually transmitted diseases (STDs) are acquired during unprotected vaginal, anal, or oral sex with an infected partner. Because STDs are contagious, their control is a serious public health concern. Proper evaluation is essential, and treatment for all sexual partners is necessary.
The risk of contracting an STD is directly related to the length of time in which a woman might come in contact with the bacteria or virus. Thus, being engaged in sexual activity from an early age increases the risk of contraction. In addition, having sex with more than one partner, or having sex with someone who has sex with more than one partner, increases the risk. Also, those women who currently have an STD or who have had one in the past are at an increased risk.
Infections with chlamydia and gonorrhea are the most common STDs, and syphilis, though it occurs less frequently in the population, is well known because it is highly contagious. All STDs can be serious if left untreated. It is recommended that women up to age twenty-six undergo annual testing for chlamydia and gonorrhea.
Both chlamydia and gonorrhea can occur in the mouth, genitals, and rectum. In most women, the initial infection site is the cervix, and from there it can spread into the uterus and fallopian tubes. Commonly, chlamydia and gonorrhea do not immediately cause bothersome symptoms, but symptoms may present up to three weeks after infection.
-
Typical symptoms include:
- Vaginal yellowish discharge
- Painful and/or frequent urination
- Burning and/or itching of the vaginal area
- Redness and swelling of the vaginal area
- Painful sexual intercourse
- Abnormal vaginal bleeding
Women experiencing any symptoms need to be evaluated by a gynecologist. Undiagnosed and untreated, chlamydia and gonorrhea can cause severe problems such as pelvic inflammatory disease (PID), an infection of the uterus, fallopian tubes and other parts of the body within the pelvis. The disease causes chills, fever, and pelvic pain. In some cases, PID may also lead to infertility. In addition, ectopic pregnancy can result from scarring of the fallopian tubes caused by PID. This condition may partially or completely block the tubes, preventing an egg released by the ovary from moving through the tubes to the uterus.
Chlamydia and gonorrhea are treated with antibiotics once diagnosed. All sexual partners must be treated as well.
Syphilis occurs in stages, and it is more easily spread in some stages than in others. Syphilis is spread by contact with a chancre, rash, wart, or infected blood. It enters the body through a cut in the skin or mucus membrane. If not treated, syphilis may affect the heart, blood vessels, and nervous system. But, if it is treated early, then the disease will cause much less damage. Syphilis first appears as a painless sore called a chancre, and it lasts anywhere from ten days to six weeks after contact with the disease. Untreated, the disease progresses to the next stage one week to three months after the appearance of the chancre, at which time a rash in the soles of the feet and the palms of the hands may appear. Flat warts may appear on the vulva, outside of the vagina. This stage frequently occurs in combination with flu-like symptoms and is highly contagious.
Syphilis diagnosis is made by examining discharge from open sores or by blood test, and it is treated with antibiotics.

Abnormal Bleeding
The uterus is a pear-shaped, muscular organ in the lower abdomen. It is wide near the top and narrow like the neck of a bottle at the bottom. The neck of the uterus is the cervix, and the lining is the endometrium. The wall of the uterus, a thick outer layer, is the myometrium – it is the muscle layer.
In women who menstruate, the endometrium thickens every month in preparation for pregnancy. If the woman does not become pregnant, the endometrial lining sheds during the menstrual period. If the woman becomes pregnant, the endometrial lining remains and serves as a surface to which the embryo implants. After menopause when menstruation stops, the endometrial lining stops the monthly process of growing and shedding. This is normal.
However, bleeding that occurs between menstrual periods or excessive bleeding during menstruation requires doctor evaluation. Such uterine bleeding can be caused by many factors. Proper evaluation is essential, followed by treatment, if appropriate.
Many young girls have episodes of irregular bleeding during the first year or two after their first menstrual cycle. This bleeding usually resolves without treatment when the hormonal cycle normalizes.
For women between adolescence and menopause, many different conditions can cause abnormal bleeding. Some women who ovulate normally experience excessive bleeding during their periods or bleed between periods. The most common causes of such bleeding are fibroids and polyps. These benign tumors are composed of uterine tissue that change the structure of the uterus and lead to irregularities. Some women do not ovulate regularly and may experience intermittent light and heavy vaginal bleeding. Fibroids and polyps can occur in these women, but there are other causes as well. Cancer and pre-cancer of the cervix or the endometrium may lead to abnormal bleeding. Other common causes include pregnancy, infections, clotting disorders, and other medical illnesses.
For women in the menopausal transition, hormonal changes can cause the endometrium to grow and produce excess tissue, increasing the chances that polyps or endometrial hyperplasia (thickened lining) will develop and lead to abnormal bleeding. Any bleeding in the menopausal years is abnormal and should be investigated. Abnormal bleeding during menopause can result from benign causes such as vaginal or uterine polyps, but cancer of the uterine lining is more prevalent in this age group.

MENOPAUSE AND HORMONAL REPLACEMENT
Menopause is the time in a woman's life during which the ovarian function declines and menstrual periods end. Most women experience menopause between the ages of forty-five and fifty-five, with the average at fifty-one. Though menopause occurs officially when it has been twelve months since the last menstrual period, the onset symptoms may start years before periods stop. The most common symptoms are irregular periods, hot flashes, night sweats, sleep problems and vaginal dryness. Mood changes are common as well. While these symptoms and changes are disruptive, effective treatments are available.
During the menopause transition, irregular periods and irregular bleeding are common, but the doctor should evaluate women in order to determine whether the bleeding is normal. If the bleeding is excessive, if it occurs more than once every three weeks, or if there is spotting between periods, women need to be evaluated.
Hormonal replacement therapy, both with traditional and bioidentical hormones, is the most effective treatment of bothersome menopausal symptoms. For most women, a combination of estrogen and progesterone is used to replace those hormones the body would have made. Although pills can be given by mouth, there are other options, and a skin patch, vaginal ring, skin gel, or cream is frequently considered a preferable method of treatment.
Hormonal replacement therapy should be taken for the shortest time period possible, usually less than five years. Women who have had breast cancer, heart disease, history of blood clots or strokes should not take hormones, and non-hormonal treatments are available in these cases.
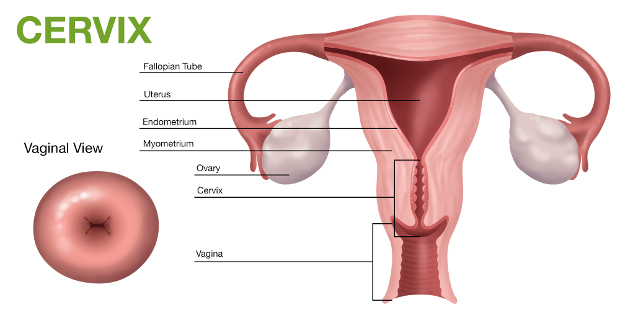
Cervix
Cervical cancer screening can detect very early changes that, if left untreated, could lead to invasive cervical cancer over the course of many years. Cervical cancer screening is performed using the Pap and HPV tests. Early detection of early abnormalities of the cells of the cervix makes treatment possible before the disease becomes invasive.
PAP TEST – HPV TEST
The Pap test is a test used to screen women for cervical pre-cancer or cancer. In women over the age of 30, testing for human papilloma virus (HPV) is performed in conjunction with a Pap test. The most important risk factor for cervical cancer is infection with the human papilloma virus. At least 80% of women are exposed to the HPV virus during their lifetime. However, most of the time the body's immune system gets rid of the virus before it does harm.
HPV is spread by direct skin-to-skin contact, including sexual intercourse, oral sex, anal sex or any other contact involving the genital area (e.g. Hand to genital contact). It is not possible to become infected with HPV by touching an object, such as a toilet seat.
It usually takes many years for HPV infection to cause cervical cancer. There are no signs or symptoms and most HPV infections are temporary and resolve within two years. When the virus persists there is a chance of developing cervical pre-cancer or cancer.
Women with abnormalities undergo further evaluation that consists of a colposcopy and biopsy. A colposcopy is an office procedure that magnifies the appearance of the cervix allowing to better see abnormalities. A colposcopy is performed similar to a pelvic examination. A speculum is used to view the cervix and the colposcope remains outside the woman's body. A biopsy of the cervix causes brief and minimal discomfort. Treatment is dependent on the results of the biopsy.
Early detection of mild abnormalities of the cells of the cervix is easily treated before the disease becomes invasive.

Breast
Breast cancer is the most common female cancer in the United States, and it is the main cause of death in women ages 45-55. Yet breast cancer can be treated effectively and cured when it is detected early. Thus, the purpose of active screening is to detect the cancer early.
There are three primary ways to screen for breast cancer: Mammogram, breast exam with your doctor, and breast self-examination. In addition, breast MRI may be recommended in addition to mammography to help find breast cancer in young women who have a high risk for developing the disease.
Mammographies are typically started in women at age forty and are performed every year thereafter. Women with higher risk factors are advised to begin mammographies earlier. If breast cancer is suspected, the region is sampled with a core needle biopsy to confirm a diagnosis. In addition to regular mammographies,clinical breast exams with the doctor improve early detection of breast cancer. The preferred examination technique includes certain motions and varying pressures, all of which are painless. Breast self-exam is helpful as an adjunct to the clinical screening tests, particularly in the detection of advanced-stage cancer, but only when proper technique is used. The doctor will show you how to self-examine the breasts properly.
Having a strong family history of breast or ovarian cancer can increase your risk of developing breast cancer. Genetic testing such as the BRCA test can identify harmful mutations in certain genes that increase the risk of breast cancer compared to the rest of the population. However, genetic testing is not perfect. In fact, most women with breast cancer or a family history of the disease do not have an abnormal gene. Plus, developing breast cancer is not a foregone conclusion even in women who test positive for an abnormal gene. The BRCA gene test is offered only to people who are likely to have an inherited mutation, based on personal or family history, or who have specific types of breast cancer.
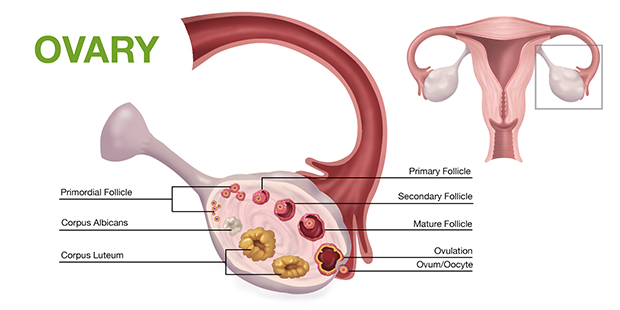
Ovary
Ovarian cancer is one of the deadliest cancers in women, in part because it is often detected at a late stage.
-
Symptoms of ovarian cancer can include:
- Urinary frequency
- Sensation of fullness or nausea
- Bloating sensation or abdominal discomfort
- Increase in size of abdomen
-
Screening tests for patients suspected of having ovarian cancer include:
- Ultrasound
- Blood tests (CA125)
Genetic counseling and BRCA gene testing should be considered in patients with a strong family history of breast or ovarian cancer.
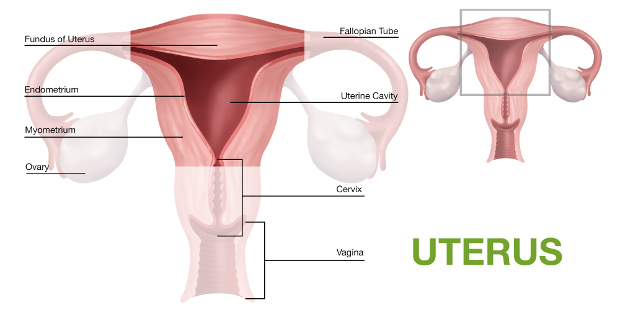
Uterus
Cancer of the lining of the uterus (endometrium) can occur in women of any age but is much more common in menopausal and obese women. The most common symptom of uterine cancer is vaginal bleeding.
-
Abnormal vaginal bleeding includes:
- Bleeding between period
- Heavy menstrual periods
- Vaginal bleeding after menopause
Evaluation of bleeding is initially performed with a transvaginal sonogram or a saline infusion sonogram. The lining of the uterus is assessed for thickness and the detection of small lesions. An endometrial biopsy or a D&C is used to obtain tissue for definitive diagnosis. Endometrial cancer detected in an early stage is potential curable with a hysterectomy.

CERVIX
Abnormality in the cells of the cervix is corrected with procedures that remove affected tissue. These procedures, which can be performed in the office or in the hospital, include LEEP or cone biopsy.
UTERUS
Symptomatic fibroids and uncontrollable bleeding at times requires surgical intervention. Minimally invasive procedures as well as open hysterectomy (removal of uterus) can be performed. Fibroids may be individually removed thus preserving the uterus. Gynecological Oncology referrals are made when uterine cancer is diagnosed.
OVARIES
When ovarian cysts require surgery, they are removed through a minimally invasive surgical procedure. Similarly, when removal of the ovaries is indicated such as in cases of positive BRCA status, a minimally invasive operation is performed. Referral to a Gynecological Oncologist of course is made if the diagnosis is malignant.
ABNORMAL BLEEDING
Bleeding abnormalities are preferably managed without surgery. The non-surgical approaches include use of medications and medicated IUDs that regulate and stop vaginal bleeding.

LABIOPLASTY (LABIA REMODELING)
Many girls and women are concerned about the appearance of their labia. Enlargement or protuberance of the labia minora can be improved with a simple office or outpatient surgical procedure. The goal of labioplasty is to create symmetrically reduced labia.
-
Patients seeking this procedure:
- Simply don't like the appearance of their labia
- Have irritation or chronic infections
- Have discomfort while playing sports
- Have pain or interference with sexual activity
- Feel that the labia actually bulges in their underwear
VAGINOPLASTY – COSMETIC VAGINAL SURGERY
Vaginoplasty is the surgical remodeling of the entrance and the walls of the vagina. This procedure improves appearance and laxity of the vagina and can be performed in the office with local anesthesia or as a hospital outpatient surgical procedure.
-
Vaginoplasty accomplishes:
- Improved aesthetic appearance of vaginal entrance and hymen
- Narrowing of the vaginal canal resulting in increased “tightness”
HYMEN
Common anatomical conditions of the hymen can lead to pain with insertion of a tampon or the inability to have intercourse. In some cases, the hymen is completely sealed, interfering with the flow of menstrual blood. These problems can be easily corrected with a simple surgical procedure in the office or the hospital.
-
 201.569.5151
201.569.5151  300 grand ave, Englewood, NJ 07631
300 grand ave, Englewood, NJ 07631
